While healthcare providers and public health departments continue to study how Stage 2 of the Electronic Health Record (EHR) Incentive Program, or “Meaningful Use,” will affect them beginning October 2013, the Health Information Technology Policy Committee has issued a Request for Comment (RFC) on proposals for Stage 3 and beyond that may shape the program after October 2015. Comments are due January 14, 2013. At least some of these proposals, shaped by comment, will re-appear in a Notice of Proposed Rule Making (and yet another round of public comment) next year.
The RFC unexpectedly pushed back a proposal for electronic case reporting of reportable conditions to an indefinite time AFTER Stage 3 (see below). Because the two Population and Public Health objectives targeted “after Stage 3” have been to focus of rapid and intensive work in the Public Health Reporting Initiative, they will likely merit further discussion as to timing.
Some items of public health interest for Stage 3 (by my own arbitrary criteria–you should read the RFC!) include:
- Adding the capability to record occupation & industry codes, sexual orientation and gender identity (optional fields) and disability status to EHR certification requirements (while not setting goals for provider capture of these elements)
- Using vital signs and lab results to support up-to-date problem lists (e.g., to use vital signs to signal potential hypertension on the problem list)
- RETIRING requirements to capture blood pressure, BMI and smoking status because recording is already at high levels (<80%, data source unstated). Progress will be tracked through hypertension and tobacco use quality measures instead.
- Increasing clinical decision support interventions from 5 to 15, including preventive services and chronic disease management, especially hypertension control and dosing of drugs for renal impairments.
- Change recording family history to recording high priority (unspecified) family history
- Educational materials made available in at least one non-English language based on which of the top-five non-English languages in US are spoken locally
- Transitions-of-care now specifically include referrals. Care summaries should include the identity of care team members like care coordinators, and EHR certification includes the ability to populate a referral form for specific referrals including smoking quit-lines.
- Notifying care coordinators (when appropriate) of significant healthcare events like emergency department visits or hospital admission or discharge.
- EHR importation and use of structured historical immunization data from immunization information systems (registries), and to receive, generate or access age-, gender-, and immunization-history-based immunization recommendations. The EHR certification criteria would requires the EHR to use standard rule sets and patient data to recommend immunization.
- Continuation without change to electronic laboratory reporting and syndromic surveillance reporting.
- Adding other mandated jurisdictional registries beyond cancer registries for which Eligible Professionals (and now Hospitals) may perform successful ongoing data submission to achieve a menu (optional) objective. In other words, cancer registries could be replaced by other registries in the menu objective for Eligible Professionals (and Eligible Hospitals would be offered a menu option for registry reporting for the first time).
- Adding a second menu option for standardized reporting to a second registry, which could include those from professional societies, public health jurisdictions or other aggregators (e.g. Accountable Care Organizations). It is a new requirement that such reporting use a national standard (“e.g., consolidated CDA”).
- Sending healthcare associated infection reports to the National Healthcare Safety Network (at least 10% of all reports sent from the certified EHR)
Two items of interest are pegged for “future stages” (i.e., after Stage 3). While it seems likely that HHS will continue to add future objectives and repairs to the program, the timing and nature of such activity is currently undefined.
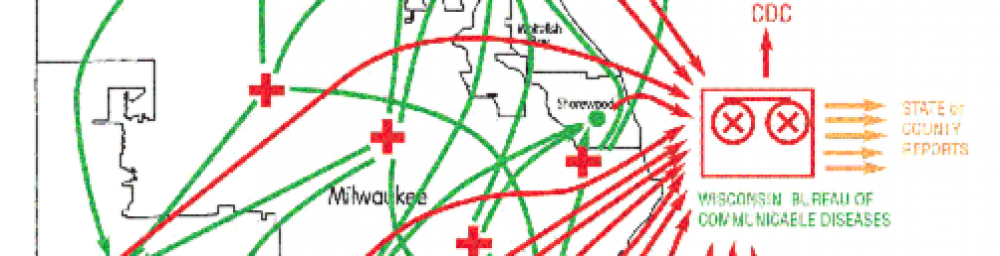
- EHRs should determine when a case report of a reportable condition need be sent to a public health agency, and should send at least 10% of initial case reports electronically. [“Case report” means clinical information on a case for which a laboratory report of a reportable condition may or may not have been sent separately. NOTE that in earlier discussions by the HIT Policy Committee this objective was slated for Stage 3.]
- Reporting of adverse event (related to, e.g., vaccines, devices, EHRs, drugs or biologics) reports to FDA and/or CDC.
Dr. Thomas Frieden, Director of the Centers for Disease Control, can see satisfaction of his request that Stage 3 tackle improved clinical hypertension control, support for tobacco quit line referrals, and bidirectional communication with immunization information systems. Other voices, inside and outside CDC, have had additional goals, and many of these are reflected as well. Some of the key questions the public health (and larger Health IT) community must answer:
- Should at least some form of public health case reporting be pushed forward into Stage 3? Will the necessary message or document standard be ready in time, AND will a meaningful number of health departments be ready to receive it? [Look for a post on this topic shortly.] Is it necessary to have a national public health knowledge system that provides rules for public health reporting, or could jurisdictional requirements be manually programmed into EHRs? And who will drive to these answers and assure needed tools are created? [Disclosure: I served as a co-chair of the Public Health Reporting Initiative for a year until September, 2012.]
- Should cancer registries be demoted to just “one of” a variety of public health disease registries?
- If a standard format is created to report to disease registries, will public health (and non-public health) registries be able to convert in time?
- Will state health departments have adapted to receiving and managing CDA documents for Cancer Registries in Stage 2, and can they apply this to other use cases (possibly case reporting or additional disease registries) for Stage 3?
- And the perennial question: will health departments be drowning in data from Stage 2, or will they successfully harness the many new ongoing data streams into more effective and efficient case management and health surveillance systems?
Answers to these questions must come in large part from health departments themselves. Many track developments using
CDC’s Meaningful Use webpage. The
Joint Public Health Informatics Taskforce of the Association of State and Territorial Health Officials, the National Association of County and City Health Officials, and seven other national public health associations, will doubtless be crafting a consensus response to RFC, and would likely welcome your thoughts as they do so.
Several more posts on Stage 2 and Stage 3 Meaningful Use objectives will follow.